Inside the ultracold freezers that will house COVID-19 vaccines
Deb BalzerDecember 10, 2020

Teams at Mayo Clinic are preparing for the anticipated arrival of COVID-19 vaccines, following federal approval. Different vaccines have different storage requirements. For instance, the Pfizer/BioNTech vaccine must be stored at minus 70 degrees Celsius (minus 94 degrees Fahrenheit) while Moderna has said that its vaccine needs to be stored at minus 20 degrees Celsius (minus 4 degrees Fahrenheit).
Mayo Clinic has multiple ultralow temperature freezers designated for vaccine storage and distribution. Each freezer can hold up to 100,000 doses of vaccine. Mayo Clinic has used these freezers for other therapeutics that have required low-temperature storage but none at such low temperatures.
Jason Christensen, Pharm.D., senior director of Pharmacy at Mayo Clinic, offers some insight into how these freezers work and will safely store the vaccines.
“What you see behind me are examples of the ultracool freezers that have been described as essential to the COVID vaccine distribution model. These freezers are capable of going down to minus 86 degrees Celsius. And for reference, that would be equivalent to minus 122.8 degrees if we were looking at it in degrees Fahrenheit.”
Watch: Jason Christensen talk about the ultracool freezers
https://youtube.com/watch?v=6yPgGqjuXLg%3Ffeature%3Doembed%26enablejsapi%3D1%26origin%3Dhttps%3A%252F%252Fnewsnetwork.mayoclinic.org
Journalists: Broadcast-quality soundbites with Christensen are available in the downloads at the end of the post as well as b-roll video of the freezers. Please “Courtesy: Jason Christensen, Pharm.D.,/Pharmacy/Mayo Clinic.”
How cold is that? For perspective, the Food and Drug Administration recommends household freezers be kept at zero degrees Fahrenheit (minus 18 Celsius) and household refrigerators at 40 degrees Fahrenheit (4 degrees Celsius).
“I have been told that on average at the South pole during the middle of winter is around negative 50 degrees Celsius. The Pfizer vaccine will be stored at minus 70 degrees Celsius, so quite a bit colder than the South pole in the middle of winter,” Christensen says.
It’s not just the ability to freeze at ultracool temperatures that makes these freezers special. Christensen explains what makes them unique.
“Outside of the large outer door, they also have smaller inner doors. Both are insulated, and these are thicker insulation than you might find in your residential freezers. And that’s all around maintaining those ultracool temperatures. Also, their compressors in circuits are designed in such a way that they cool not only the chamber, but the critical compressor components all around, minimizing heat generation.”
Being able to monitor temperature control is another aspect of the freezers.
“What you notice on the doors is temperature monitoring that’s built into the freezer itself,” says Christensen. “In addition, we will have wireless temperature monitors that communicate over Wi-Fi for continuous 24/7 temperature monitoring. A third redundancy is a data logger that is housed within the unit itself. If something happened with the alerting on the unit, or the continuous 24/7 monitoring that we have in place, we will also have a data logger within the unit so that we can validate the temperatures that were maintained during that time.”
For the safety of its patients, staff and visitors, Mayo Clinic has strict masking policies in place. Anyone shown without a mask was recorded prior to COVID-19 or in an area not designated for patient care, where social distancing and other safety protocols were followed.
Information in this post was accurate at the time of its posting. Due to the fluid nature of the COVID-19 pandemic, scientific understanding, along with guidelines and recommendations, may have changed since the original publication date.
For more information and all your COVID-19 coverage, go to the Mayo Clinic News Network and mayoclinic.org.
Related Articles
Pfizer decision to turn off temperature sensors forced scramble to ensure Covid-19 vaccines kept ultra-cold
Olivia GoldhillDec. 17, 2020

A last-minute snafu this fall threatened to disrupt the smooth rollout of the first Covid-19 vaccine approved in the United States, according to industry officials.
At issue was how to monitor the temperature of the ultra-cold storage containers being used to distribute vials of the vaccine developed by Pfizer and its partner BioNTech. Pfizer, the officials told STAT, planned to disconnect temperature-monitoring sensors on the containers once they were delivered to health care providers — though many of the providers needed to use the boxes to store the vials for up to 30 days. Without the monitoring systems, providers would have no way of knowing if the vials had thawed prematurely, rendering the vaccine unusable.
In the end, the U.S. government’s Operation Warp Speed scrambled to address the problem, signing a $25 million deal in mid-November with Controlant Global, an Icelandic company that created the proprietary temperature-monitoring platform for all Pfizer’s shipping containers. Under this agreement, Pfizer will discontinue its temperature monitoring once the boxes arrive at their destination, and the federal government will simultaneously turn the system back on.
Still, the episode highlights how, in the frenzy to get a vaccine to the public, details crucial to its distribution were overlooked until late in the game. And it reflects how, despite efforts to protect vaccine makers from liability, legal concerns are shaping their actions. Experts said concerns over legal action, as well as bad publicity if vaccine doses were lost to thawing after delivery, likely drove Pfizer’s thinking.
Pfizer is shipping its vaccines in special containers packed in dry ice to keep them at the required minus-70 degrees Celsius. As few freezers get that cold, many health systems are using these containers to store the vaccines after they arrive. Premier, a group purchaser for U.S. hospitals, said that it asked Pfizer in November to reconsider its decision to disconnect the sensors, and that for weeks, health care providers sought to clarify whether they would need to purchase their own temperature sensors.
“These vaccines need to be maintained at a specific temperature to ensure they stay viable. When holding vaccines in a cooler and refreshing with dry ice, it’s hard to know if you’re maintaining the temperature,” said Jessica Daley, vice president of strategic supplier engagement at Premier.
It’s fairly unusual for temperature-monitoring devices to go to ultra-low temperatures, and Daley said there weren’t enough alternatives available to replace those that Pfizer turned off. It was only in early December that Premier and providers learned that Operation Warp Speed (OWS) had resolved the problem, said Premier’s director of advocacy, Soumi Saha.
Neither Pfizer, Controlant, nor the Trump administration would explain exactly how the monitoring handoff works. “Pfizer will de-activate the temperature monitor on their shipping container once they are delivered. Operation Warp Speed contracted with the manufacturer of the device to immediately re-activate it with no loss of temperature monitoring and no loss of data,” Natalie Baldassarre, a spokeswoman for the Department of Health and Human Services, said in a statement.
The contract makes clear that OWS had little choice but to pick up responsibility. “As Pfizer will only monitor the temperature through transportation and up to Government acceptance, the Government requires the ability to monitor the vaccine … until the vaccine has been utilized and the shipping containers returned to Pfizer,” reads the contract.
Operation Warp Speed only started market research into temperature-monitoring for the boxes on Nov. 9, according to the Controlant agreement, though the government signed a $1.95 billion contract with Pfizer to provide 100 million doses of the vaccine in July.
The late-stage contract with Controlant suggests that this issue wasn’t fully thought through when the U.S. government signed the contract with Pfizer, said Ameet Sarpatwari, assistant professor of medicine at Harvard Medical School.
“Somewhere the ball got dropped,” he said. “Instead of turning off [the monitoring system], turning back on, it could have just been a continuous process. From a safety standpoint, that seems to be a better way to go.”
He said the original contract with Pfizer could have left room for discussions over who would have oversight of maintaining the ultra-cold temperatures. “A bit more of a systematic process that included transparency could have secured input from others that would have shown some details were insufficient with this contract,” said Sarpatwari. “Rather than being forced upon us, it could have been a decision of how we want to allocate that burden.”
Pfizer did not respond to requests to explain why it decided to disconnect the remote temperature monitoring devices. The company “is working very closely with Operation Warp Speed (OWS) on ensuring a temperature monitoring solution for points of uses if our thermal shipper is the chosen method for frozen storage,” spokesperson Amy Rose wrote in an email.
The problem is unique to Pfizer’s vaccine. The Moderna vaccine expected to receive emergency authorization later this week can be stored in most standard freezers, and is stable for 30 days at refrigerated temperatures. Only Pfizer’s shot requires such ultra-cold storage that doses will be kept in the containers they’re shipped in.
Neither the U.K. nor Canada has faced the issue yet. In both countries, the first Pfizer vaccines are being sent to sites equipped with ulta-cold freezers, so the shipping containers will not be used for storage after delivery.
In the U.S., once Pfizer had a signed supply contract with OWS, there was no reason for the company to go beyond what the terms require, said bioethicist Arthur Caplan, of New York University. “There’s way too much risk there, which they don’t need,” said Caplan. “If I’m Pfizer, I’ve sold my vaccine, I’ve made it, I’ve shipped it to where you told me, I’m not in the rest of these businesses, and I don’t care.”
Vaccine manufacturers and distributors are protected from liability claims under the Public Readiness and Emergency Preparedness (PREP) Act. But several experts say that, despite these protections, Pfizer may well have acted from a fear of repercussions.
“How much can Pfizer do? They don’t have their staff there,” said Mark Capofari, who was director of global logistics at Merck from 1995 to 2007 and currently lectures on supply chain management at Penn State University. “I don’t know if any company would want to be liable from that point forward.”
Given the lack of control Pfizer has once a vaccine reaches its destination, continuing to monitor temperature would bring unnecessary added risks. “It’s the job of the lawyers to anticipate potential claims,” said Dorit Reiss, law professor at the University of California, Hastings College of the Law, whose research focuses on vaccines.
Efforts to avoid liability tend to create inefficiencies and slow down the process, which the PREP act was intended to mitigate. The plan to change ownership of the temperature monitoring system “is only going to lead to disruptions and problems,” said Lawrence Gostin, a professor of global health law at Georgetown University. “It’s not efficient and reliable. And it’s unnecessary.”
Concerns over its public image could also have pushed Pfizer to disentangle itself from temperature monitoring at the final stage of vaccine storage. The company has garnered tremendous positive publicity through its quick development of a Covid-19 vaccine, and has an interest in protecting this reputation. “There could be publicity issues,” said Robert Field, professor of law and health management and policy at Drexel University. “If they’re concerned problems could occur at the end point, the pharmacy or wherever injections occur, they wouldn’t want to be associated. They may feel it’s not in their comfort zone, that’s not their expertise.”
Companies are naturally risk-averse and, having created a vaccine, there’s little benefit to Pfizer in continuing to keep track of vaccine storage standards beyond the delivery date. “It’s wiping your hands of accountability. You don’t want to be blamed legally or publicly, you don’t want to be held accountable and so push it over to some other entity, in this case the government,” said Gostin. “History teaches us that companies will try to protect themselves and the bottom line at any cost. Any time they can push off responsibility, whether it’s to a government or a hospital or private hospital or to a doctor’s office or pharmacy, they will.”
23 HCOS prepares for Pfizer vaccines
The ultra-low temperature freezer for the Pfizer vaccines arrived at Moody Air Force Base, Georgia, Sept. 1, 2021. Due to the specifications, the vaccines’ temperature needs to stay at minus 80 degrees Celsius to remain viable for administration. (U.S. Air Force photo by Senior Airman Rebeckah Medeiros)
Manufacturing and Distributing the COVID-19 Vaccine
Pfizer consistently and diligently monitors the supply of our medicines. We operate one of the most sophisticated supply chain systems in the industry, with over 35 Pfizer-owned sites and over 300 suppliers globally, which provides capacity and redundancy as needed. Our manufacturing and supply chain professionals have been working non-stop to ensure that the global supply of Pfizer medicines continue to be available to patients. We have implemented an unprecedented and comprehensive preparedness plan to control our site operations and will continue to provide timely updates if there is any new information to be shared.
A Cold Chain Overview
with Angela Hwang, Group President, Pfizer Biopharmaceuticals Group
Cold Chain Distribution
How is the cold chain distribution for the Pfizer and BioNTech investigational vaccine being managed?
A Look at Cold Storage & Distribution
with Mike McDermott, Chief Global Supply Officer, Executive Vice President
A Look at Cold Storage & Distribution
with Mike McDermott, President, Pfizer Global Supply
- Where is the Pfizer-BioNTech COVID-19 vaccine made?Pfizer and BioNTech are continuing to leverage a global supply chain and manufacturing network that spans four continents and includes more than 20 facilities.
- How is the Pfizer-BioNTech COVID-19 vaccine being distributed?Pfizer has activated its extensive U.S. and European manufacturing network, including thousands of highly skilled U.S. workers in multiple states and localities, to prepare to produce the COVID-19 vaccine. We currently have the capacity to produce 4 billion doses annually, pending demand.
- What is the path of a vaccine from Pfizer’s facilities to where it’s distributed to patients?We have developed detailed logistical plans and tools to support effective vaccine transport, storage and continuous temperature monitoring. Our distribution is built on a flexible just-in-time system which will ship the frozen vials to the point of vaccination.Our distribution approach will be to largely ship from our Kalamazoo and Puurs sites direct to the point of use (POU). However, we will also be using our existing distribution centers for the COVID-19 distribution in Pleasant Prairie, WI and in Karlsruhe, Germany. These distribution centers will have a dedicated area designated to store product that is not going direct from our Kalamazoo or Puurs sites to POU.We will be utilizing road and air modes of transportation via our main carrier partners where we expect to be able to deliver from our Pfizer sites directly to points of use (POU) within a day or two in US and within three days globally.
- How will Pfizer maintain vaccine integrity during distribution?Pfizer is a proven, reliable multinational vaccine producer, supplying vaccines to more than 165 countries. Today, Pfizer manufactures more than 200 million doses of Pfizer vaccines annually and is one of the largest sterile injectables suppliers in the world, producing more than 1 billion sterile units per year. We have experience working with customers in all markets to ensure success.We have years of proven experience in supply chain and cold chain management, and we are accelerating the development of innovative technologies to further advance our capabilities as a supply chain leader.Our track record gives us confidence in our ability to quickly scale and manufacture and distribute large quantities of a high-quality COVID-19 vaccine, leveraging multiple sites in the US and Europe.We have also developed packaging and storage innovations to be fit for purpose to meet the needs of our global network.We have developed detailed logistical plans and tools to support effective vaccine transport, storage and continuous temperature monitoring. Our distribution is built on a flexible just-in-time system which will ship the frozen vials to the point of vaccination.The intent is to utilize Pfizer-strategic transportation partners to ship by air to major hubs within a country/region and by ground transport to dosing locations.
- What is a “cold chain”? “Cold chain” is how the temperature of perishable products are managed in order to maintain quality and safety from end to end in the distribution process. Cold chain is used for consumer products like ice cream and other frozen foods, as well as medicines and vaccines.
- How is Pfizer utilizing a cold chain process to distribute its vaccine?We have developed packaging and storage innovations to be fit for purpose to meet the needs of our global network. We have specially designed, temperature-controlled thermal shippers utilizing dry ice to maintain recommended temperature conditions for up to 10 days unopened. The intent is to utilize Pfizer-strategic transportation partners to ship by air to major hubs within a country/region and by ground transport to dosing locations.
- How can you prevent a cold chain failure?We have specially designed, temperature-controlled shippers utilizing dry ice to maintain recommended temperature conditions up to 10 days unopened. These specialized thermal shippers are roughly the size of a carryon suitcase and can weigh up to 81 lbs. fully loaded.We will utilize GPS-enabled thermal sensors in every thermal shipper with a control tower that will track the location and temperature of each vaccine shipment across their pre-set routes. These GPS-enabled devices will allow Pfizer to proactively prevent unwanted deviations and act before they happen.
- How do hospitals and pharmacies keep vaccines cold?Once a POU receives a thermal shipper with our vaccine, they have three options for storage:
- Ultra-low-temperature freezers, which are commercially available, can extend shelf life for up to 18 months.
- The Pfizer thermal shippers, in which doses arrive, can be used as temporary storage units by refilling with dry ice every five days for up to 30 days of storage.
- Refrigeration and freezer units are commonly available in hospitals and pharmacies. The vaccine can be stored for up to 10 weeks at refrigerated 2-8°C conditions, the standard temperature of a refrigerator.
For additional information about Pfizer, please see our filings with the U.S. Securities and Exchange Commission, including the information provided in the sections captioned “Risk Factors” and “Forward-Looking Information and Factors That May Affect Future Results”.
Pfizer-BioNTech COVID-19 Vaccine has not been approved or licensed by FDA, but has been authorized for emergency use by FDA, under an EUA to prevent Coronavirus Disease 2019 (COVID-19) for use in individuals aged 6 months through 11 years of age. The emergency use of this product is only authorized for the duration of the declaration that circumstances exist justifying the authorization of emergency use of the medical product under Section 564(b) (1) of the FD&C Act unless the declaration is terminated or authorization revoked sooner.
23 HCOS prepares for Pfizer vaccines
Sept. 10, 2021
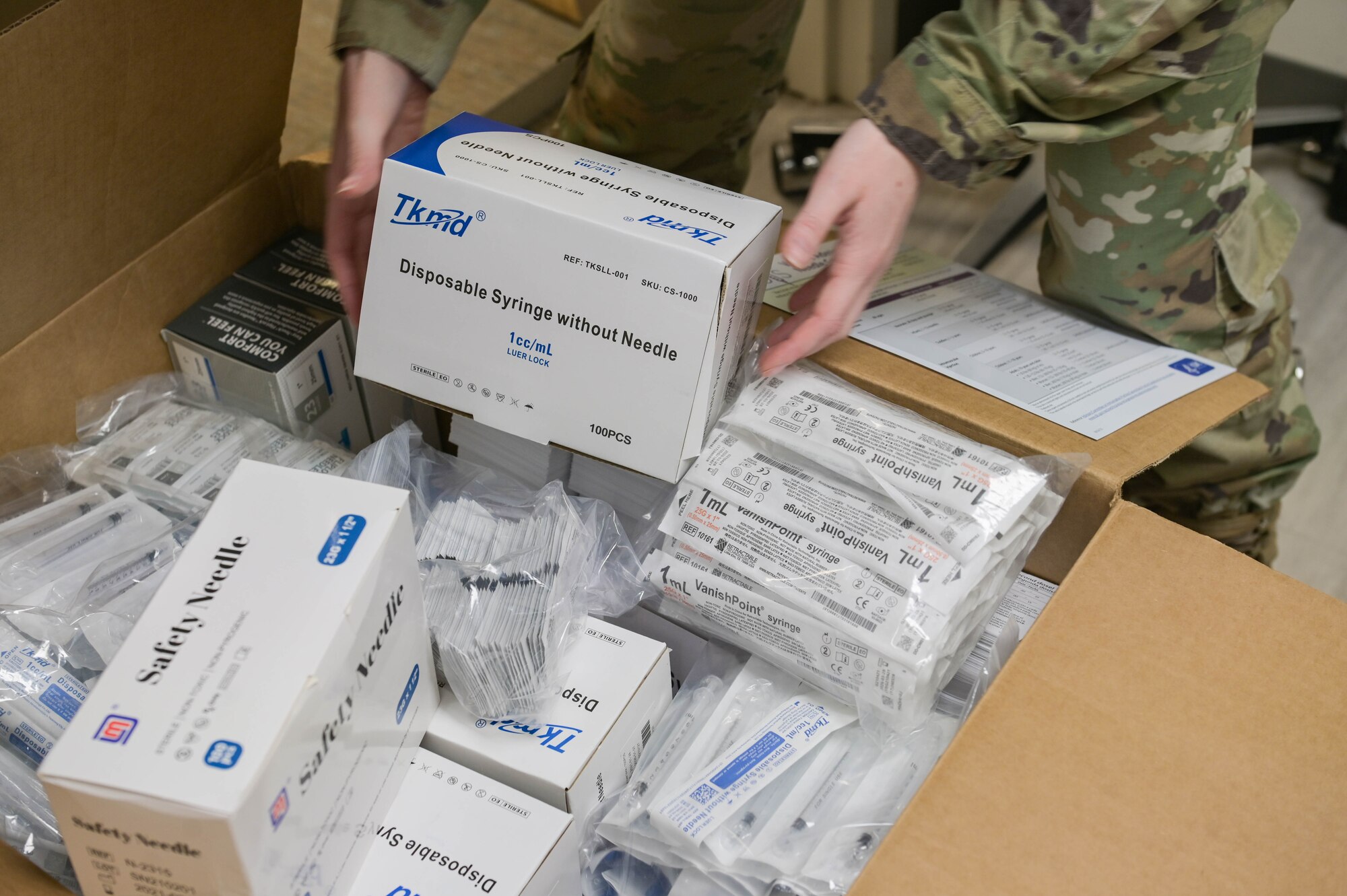
The 23rd Health Care Operations Squadron at Moody Air Force Base, Georgia, received a freezer capable of housing the Pfizer vaccine along with 1,170 doses of the vaccine with additional replenishment orders pending approval, Sept. 4 2021.
Secretary of Defense Lloyd J. Austin III published a vaccine mandate on Aug. 24, 2021, making the COVID-19 Food and Drug Administration (FDA) approved vaccines mandatory for all U.S. military servicemembers. Currently Pfizer is the only FDA approved COVID-19 vaccine.
“The 23rd Medical Group immunizations team has received 1,170 Pfizer doses and the freezer to immunize the Moody AFB community,” said Staff Sgt. Casey Rowe, 23rd Health Care Operations Squadron allergy and immunizations technician. “We received the Pfizer freezer on Sept. 1, 2021 and the vaccines on Sept. 4, 2021. Our medical logistics team came in on that Saturday to ensure the vaccines maintained proper cold chain management temperature threshold.”
Due to its specifications, the vaccine needs to be housed at a temperature of minus 80 degrees Celsius to stay viable for administration.
“With this vaccine, we are ensuring Moody is ready to deploy all of our active-duty members anywhere at any time, that way they can do the best job possible while being protected against the COVID-19 virus during this pandemic,” Rowe said.
The 23rd HCOS will be conducting a Pfizer Mass Vaccination Clinic on Sept. 17, 2021, for active-duty personnel only from 6 a.m. to 10 p.m. The 23rd MDG will begin offering appointments and administering the Pfizer vaccine to the Moody community on Sept. 20, 2021. Pfizer vaccination clinic appointments will be available every Monday, Wednesday and Friday afternoon.
“We are so excited to administer the Pfizer vaccine to the Moody AFB community to aid in the protection against the COVID-19 virus and protection of the local community,” Rowe said.
For more information on the Pfizer vaccine, please visit https://www.fda.gov, and to schedule a vaccine, visit https://www.vaxmoody.com.
